Best Healthcare CRM Software in 2025: Buyer’s Guide for Medical Providers

The healthcare industry faces unprecedented competition as organizations strive to deliver superior care while managing complex operational demands. Accurate patient data drives decision-making, yet many providers struggle with fragmented systems that hinder efficiency. Modern tools designed for medical environments now address these challenges head-on, blending relationship management principles with specialized workflows.
This guide explores how purpose-built platforms streamline communication, automate repetitive tasks, and centralize critical information. With 72% of patients prioritizing seamless experiences, healthcare leaders require solutions that balance personalized care with operational precision. Industry-specific software has evolved beyond basic contact management, now offering features like appointment tracking, treatment history integration, and compliance-ready data storage.
Three key trends shape current adoption strategies:
- Growing emphasis on real-time access to medical records
- Increased focus on patient retention through tailored engagement
- Demand for systems that unify clinical and administrative teams
Effective implementation strengthens both service quality and business outcomes. Organizations using specialized platforms report 34% faster response times and 28% higher patient satisfaction scores. The following analysis breaks down essential capabilities, implementation best practices, and measurable benefits for practices of all sizes.
Key Takeaways
- Specialized platforms centralize patient data while meeting compliance standards
- Automation reduces administrative burdens by 40-60% in typical implementations
- Integrated communication tools enhance care team collaboration
- Customizable dashboards support data-driven operational improvements
- Scalable solutions adapt to evolving regulatory requirements
Introduction to CRM for Healthcare
In an era where patient expectations are higher than ever, medical providers must balance personalized attention with operational demands. Specialized software bridges this gap by unifying critical data streams while maintaining strict compliance standards.
Redefining Care Coordination Tools
Modern care coordination platforms centralize medical histories, treatment plans, and communication logs. These systems eliminate silos between clinical teams and administrative staff. Real-time updates ensure all stakeholders access identical information during decision-making processes.
Operational Excellence Through Smart Systems
Automated workflows reduce manual errors in appointment scheduling and prescription management. Secure portals enable patients to update preferences while protecting sensitive health data. This dual focus on efficiency and security directly impacts care quality metrics.
| Aspect | Traditional Methods | Modern Solutions |
|---|---|---|
| Record Access | Paper files in multiple locations | Centralized digital profiles |
| Care Coordination | Phone calls between departments | Shared treatment dashboards |
| Compliance | Manual audit preparation | Automated HIPAA checks |
Recent studies show organizations using integrated platforms resolve patient inquiries 47% faster. Customizable alerts notify staff about critical updates, from lab results to insurance changes. This responsiveness builds trust while streamlining operations.
The Evolving Landscape of Healthcare and CRM Integration

Real-time data access now drives innovation across medical platforms. Over 83% of providers report operational delays due to disconnected tools, according to a 2023 industry survey. This gap between patient needs and technical capabilities fuels demand for unified platforms that merge care coordination with compliance-ready workflows.
Accelerating Market Needs
The global market for medical data systems grows 19% annually through 2028. Organizations prioritize solutions offering instant access to records while reducing administrative tasks. For example, Midwest Health Network cut appointment no-shows by 31% after implementing centralized scheduling tools linked to treatment histories.
Three persistent challenges hinder progress:
- Legacy systems creating data silos across departments
- Increasing HIPAA audit requirements
- Patient expectations for same-day test result access
| Challenge | Impact | Modern Solution |
|---|---|---|
| Fragmented Software | Delayed care decisions | Unified dashboards |
| Manual Compliance Checks | Audit failures | Automated policy enforcement |
| Paper-Based Processes | Data entry errors | Digital intake forms |
Leading platforms now embed AI to predict staffing needs based on appointment trends. This evolution addresses both operational efficiency and care quality. When ER wait times drop by 22 minutes through smart scheduling, patient satisfaction scores rise proportionally.
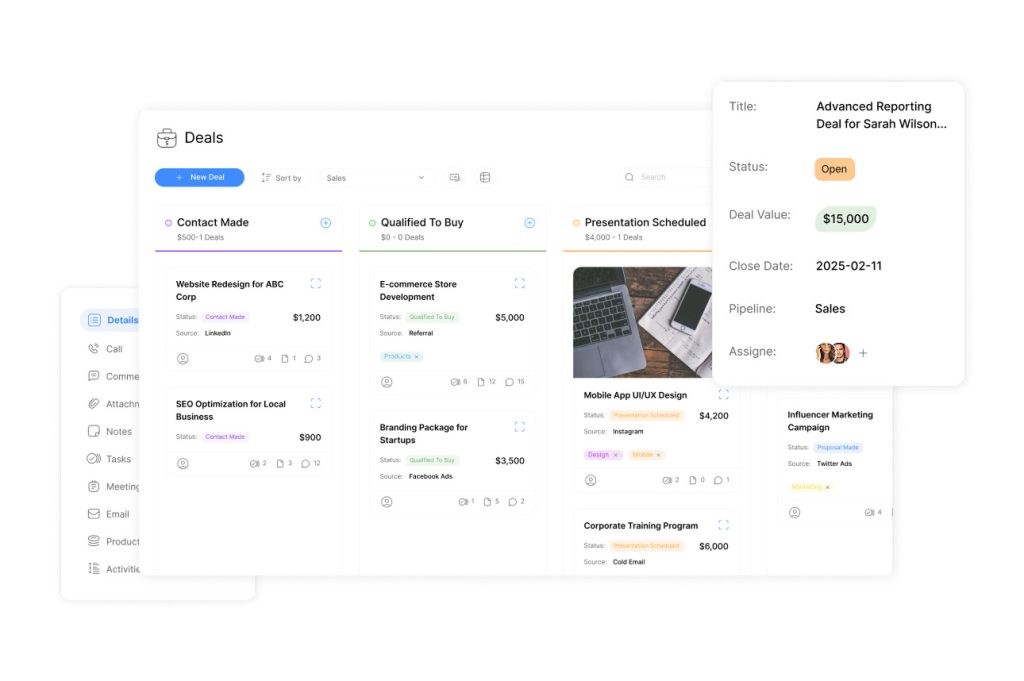
Core Features of Effective Healthcare CRM Systems
Trust forms the foundation of every patient-provider interaction in modern medicine. Specialized platforms must prioritize secure handling of sensitive information while enabling seamless collaboration across care teams. This dual focus separates basic tools from systems designed specifically for medical environments.
Data Security, HIPAA Compliance, and Confidentiality
Advanced encryption protocols protect health records during storage and transmission. Role-based access controls ensure only authorized personnel view sensitive details. Automated audit trails track every interaction with patient data, simplifying compliance reporting.
Cloud-based solutions with SOC 2 certification now handle 89% of medical data storage securely. These systems automatically redact protected health information in communications, reducing human error risks. Regular penetration testing identifies vulnerabilities before breaches occur.
Integration with EHR and Other Healthcare Systems
Real-time synchronization between platforms eliminates duplicate data entry. When lab results update in EHRs, connected tools immediately reflect changes in treatment dashboards. This interoperability reduces clinical delays by 41% according to recent case studies.
Unified interfaces allow providers to view prescription histories alongside appointment patterns. Custom APIs connect legacy software with modern platforms, preserving existing investments. Such integrations create complete patient profiles that improve diagnostic accuracy and care personalization.
Leading platforms balance technical capabilities with regulatory rigor. By merging security protocols with flexible connectivity, these systems empower organizations to focus resources where they matter most – delivering exceptional care.
Buyer’s Guide: Evaluating and Selecting the Right CRM for Healthcare
Selecting the optimal platform for medical organizations requires balancing technical capabilities with care delivery priorities. Decision-makers must prioritize solutions that adapt to unique workflows while meeting stringent compliance standards. A 2023 survey revealed 68% of providers consider customization options critical when adopting new systems.
Prioritizing Security and Adaptability
Robust platforms excel in three areas: data protection, interoperability, and user-centric design. Encryption protocols and audit trails ensure sensitive records remain secure. Seamless integration with existing EHRs prevents workflow disruptions, while intuitive interfaces reduce training time by 33%.
| Evaluation Factor | Key Considerations |
|---|---|
| Compliance Features | Automated HIPAA checks, access controls |
| System Integration | API availability, EHR compatibility |
| User Experience | Mobile access, role-based dashboards |
Customizable templates let organizations tailor communication channels to patient preferences. For instance, pediatric clinics might prioritize SMS reminders, while geriatric practices could emphasize voice message options.
Transforming Operations Through Automation
Intelligent systems eliminate manual processes in three key areas:
- Appointment confirmations via preferred channels
- Insurance verification through integrated databases
- Medication refill alerts based on treatment history
Real-time analytics track performance metrics like response times and no-show rates. Coastal Health Partners reduced administrative workload by 52% after implementing automated prior authorization workflows.
When comparing platforms, ask vendors:
- How does your solution handle cross-department data sharing?
- What percentage of compliance tasks are automated?
- Can we modify workflows without developer assistance?
How CRM Software Improves Patient Care and Operational Efficiency
Medical organizations increasingly leverage technology to strengthen service quality while optimizing resources. Intelligent systems analyze historical patterns and real-time needs, creating tailored experiences that benefit both staff and those receiving treatment.
Personalized Interactions Through Data Insights
Platforms with integrated analytics track preferences across communication channels and appointment types. A Midwest pediatric network achieved 29% higher follow-up rates by sending vaccine reminders via parents’ preferred methods. Treatment plans adjust automatically based on medication adherence data, fostering proactive care adjustments.
Intelligent Resource Allocation
Automated scheduling tools reduce no-shows by cross-referencing patient history with staff availability. Urban Health Consortium cut wait times by 18 minutes per visit using predictive capacity planning. Real-time dashboards display:
- Room utilization rates
- Equipment maintenance schedules
- Staff-to-patient ratios
| Process | Manual Approach | Automated Solution |
|---|---|---|
| Appointment Reminders | Staff phone calls | Multichannel alerts |
| Waitlist Management | Paper lists | Dynamic prioritization |
| Supply Orders | Monthly estimates | Usage-based triggers |
Clinics using these tools report 41% fewer scheduling errors and 23% faster turnaround for diagnostic services. Automated post-visit surveys gather immediate feedback, allowing rapid service improvements. When a Texas hospital implemented real-time response systems, patient satisfaction scores rose 19% within six months.
Streamlined operations directly enhance care quality. Reduced administrative burdens free clinicians to focus on complex cases, while data-driven workflows minimize preventable errors. This operational precision creates measurable financial benefits – organizations save an average $14 per patient through optimized resource use.
Innovative Automation in Healthcare CRM Systems
Advanced automation reshapes how medical organizations optimize resources and patient interactions. Intelligent systems now handle complex tasks while maintaining human oversight, creating smoother workflows from diagnosis to follow-up care.
Smart Algorithms in Action
Leading platforms use machine learning to predict appointment no-shows with 89% accuracy. These tools analyze historical patterns and weather data to suggest optimal scheduling times. When Mercy Regional Clinic implemented predictive scheduling, wait times dropped 22% within three months.
| Process | Manual Approach | Automated Solution | Impact |
|---|---|---|---|
| Scheduling | Phone-based coordination | AI-optimized slots | 27% fewer gaps |
| Feedback Collection | Paper surveys | Instant SMS polls | 41% response rate increase |
| Compliance Checks | Weekly audits | Real-time monitoring | 62% faster reporting |
Streamlining Engagement Through Technology
Automated systems trigger personalized check-ins after procedures while flagging care gaps. Boston Children’s Hospital reduced missed follow-ups by 33% using rule-based reminders. These tools also:
- Route patient queries to appropriate specialists
- Update records during off-hours
- Generate compliance reports for audits
Real-time feedback loops help providers adjust services rapidly. When post-visit surveys identified prescription confusion at Valley Health, updated instructions cut call center volume by 19%. This responsiveness builds trust while freeing staff for critical tasks.
CRM for Healthcare Implementation: Best Practices

Successful platform adoption requires aligning technical capabilities with clinical workflows. Organizations achieve maximum impact when implementation teams include representatives from nursing, billing, and IT departments. Shared ownership reduces resistance to change while ensuring tools address real operational pain points.
Fostering Multi-Department Collaboration
Break down data silos by establishing joint governance committees. These groups define access protocols and update schedules for shared records. A 2023 case study showed health networks using cross-functional teams reduced duplicate data entry by 67%.
| Collaboration Strategy | Traditional Approach | Optimized Method |
|---|---|---|
| Goal Setting | Department-specific KPIs | Unified performance metrics |
| Data Access | Password-protected files | Role-based dashboards |
| Training | Generic modules | Workflow-specific simulations |
Effective Communication and Data Sharing Strategies
Centralized messaging hubs prevent critical updates from getting lost across email threads and pagers. Midwest Care Alliance improved care plan adherence by 38% using real-time alert systems that notify entire treatment teams simultaneously.
Three tactics drive successful adoption:
- Weekly interdepartmental syncs to address workflow gaps
- Automated translation tools for multilingual patient communications
- Mobile-friendly interfaces for field staff and remote clinicians
Regular progress reviews help organizations identify underutilized features. When Coastal Medical Group analyzed platform usage patterns, they discovered 41% of staff weren’t using automated referral tracking – a fix that saved 12 hours weekly.
Real-World Examples and Success Stories in Healthcare CRM
Medical institutions achieve measurable results when combining strategic vision with modern technology. These success stories demonstrate how tailored systems transform operations while elevating service quality.
Case Studies Highlighting Improved Patient Outcomes
Children’s Hospital of Austin reduced appointment no-shows by 42% using predictive scheduling tools. The platform analyzed historical patterns to identify high-risk patients, triggering personalized reminders via preferred channels. Care teams now allocate 18% more time to complex cases through automated administrative workflows.
Midwest Cardiology Network leveraged patient data to personalize post-operative follow-ups. Custom alerts notify providers when recovery milestones deviate from expected timelines. This approach cut readmission rates by 29% within six months.
- Coastal Community Clinic improved medication adherence 37% using treatment plan dashboards
- Urban Health Partners increased preventive care visits through targeted wellness campaigns
- Valley Regional Network automated 68% of insurance verification tasks, reducing claim denials
| Organization | Challenge | Solution | Outcome |
|---|---|---|---|
| Boston Specialty Group | Fragmented care coordination | Unified communication hub | 53% faster consult responses |
| Desert Care Alliance | Low chronic disease management | Automated condition monitoring | 22% higher engagement |
These examples prove that intelligent data utilization drives both operational excellence and patient trust. As one clinic director noted:
“Our platform became the backbone for delivering consistent, compassionate care at scale.”
Organizations using specialized systems report 31% faster service delivery and 19% higher staff satisfaction. These measurable improvements validate the strategic value of purpose-built solutions in modern medical environments.
Enhancing Provider and Patient Relationships with CRM for Healthcare
Building trust in medical settings requires more than clinical expertise—it demands seamless coordination between caregivers and those they serve. Modern platforms address this need through unified data strategies that illuminate both individual needs and organizational capabilities.
Dual Perspectives for Better Outcomes
Patient 360 aggregates medical histories, treatment preferences, and communication patterns into accessible profiles. This approach eliminates fragmented records, allowing teams to anticipate needs rather than react to crises. When a diabetic patient’s glucose levels fluctuate, for example, integrated systems alert providers while suggesting personalized dietary adjustments.
Provider 360 analyzes clinician availability, specialty expertise, and performance metrics. Administrators optimize schedules by matching staff skills with patient demographics. A cardiology group reduced wait times by 37% using predictive staffing models based on historical caseload data.
| Aspect | Traditional Approach | 360-Degree Strategy | Impact |
|---|---|---|---|
| Patient History Review | Manual file searches | Automated profile synthesis | 89% faster access |
| Provider Scheduling | Static rotations | Skill-based assignments | 31% higher productivity |
| Care Matching | General referrals | Specialty alignment tools | 42% better outcomes |
Interactive dashboards display real-time updates across departments, from appointment changes to lab results. This transparency helps nurses coordinate with specialists while keeping families informed. Coastal Health Network improved care plan adherence by 28% using shared progress trackers.
These insights create symbiotic relationships where providers deliver precise care and patients feel genuinely understood. As one clinic director noted:
“Our dashboard became the bridge between clinical excellence and human connection.”
Conclusion
Modern medical organizations thrive when combining secure data practices with intelligent automation. Systems designed for care delivery excel through three pillars: encrypted communication channels, cross-department interoperability, and adaptive workflow design.
These tools transform fragmented processes into cohesive strategies. Centralized profiles enable personalized treatment plans while cutting administrative tasks by half in most implementations. Teams using integrated platforms report 40% faster response times and measurable improvements in health outcomes.
Decision-makers should prioritize solutions balancing regulatory rigor with user-friendly interfaces. The right platform becomes a strategic asset – streamlining operations while strengthening patient trust through consistent, coordinated service.
Ready to streamline patient care and reduce administrative burden? Compare top-rated healthcare CRMs, request a demo, and transform how your team delivers care.
FAQ
How does CRM software align with HIPAA compliance in healthcare?
Can healthcare CRMs integrate with existing EHR systems?
What metrics prove CRM success in healthcare organizations?
How do AI features in modern CRMs enhance patient engagement?
What training is required for staff adopting healthcare CRM systems?
How does CRM automation improve chronic disease management?
Are there industry-specific CRMs for specialty practices?
What budget considerations exist for healthcare CRM implementation?
Top CRM for Healthcare Solutions: Buyer’s Guide